Eyelid Skin Cancer Surgery And Eyelid Reconstruction
The eyelid skin is the thinnest skin on the body with significant long-term exposure to sunlight. That makes the eyelids one of the most common locations on the body to develop benign and cancerous skin lesions. Luckily, most eye fold lesions are benign and easily treated by simple excision. The most common eyelid cancer types are basal cell carcinoma and squamous cell carcinoma. The symptoms could be a subtle bump, non-resolving “sty” or lesion, lash loss, or ulcerating non-healing nodule. presence of a nodule or lesion on the eye fold that grows, bleed or ulcerates should be evaluated. The diagnosis is made by examination and biopsy.

Skin Cancer Overview
Basal cell carcinomas are the most common eyelid skin cancer. They grow slowly and steadily but don’t metastasize. Squamous cell carcinomas are the second most common eyelid skin cancer and behave similarly to basal cell carcinomas but are usually more aggressive. Melanoma of the eye fold skin are very rare but have the same prognosis as other body melanomas and need to be treated aggressively.
Basal Cell Carcinoma
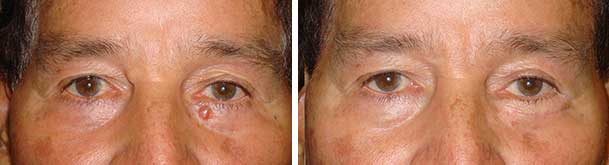
Basal cell tumors represent the ninety percent of eyelid tumors. These skin cancers grow slowly over months and years. They most often appear as a pearly nodule that eventually starts to break down and ulcerate. Despite being a cancer, these tumors don’t spread to distant areas but rather just continue to grow and infiltrate the surrounding tissue. They typically can be cured by simple excision followed by reconstruction of the defect left behind after the tumor removal.
Squamous Cell Carcinoma and Melanoma
These types of tumors occur much less common but are more aggressive and require more involved care to ensure complete treatment. Again, primary treatment involves removing the tumor, but care must also be taken to ensure the tumor has not spread anywhere, causing larger health problems. Your surgeon will help coordinate this as part of your treatment depending on the size and circumstances of the tumor at presentation.
Article Published by Los Angeles’ Dr. Taban about Eyelid Reconstruction Using Bilobed Flap
Treatment (Eyelid skin cancer surgery, Mohs Eyelid Reconstruction)
The goals of skin cancer surgery are three fold: 1) To remove all the tumor, 2) To reconstruct an eyelid where it can properly close and protect the eyeball, and 3) To achieve the best cosmetic surgery outcome. An eye fold skin cancer surgeon specialist needs to understand these important goals.
Eyelid cancers are usually slow growing, however, because there is very little eye fold tissue to begin with, it is best to excise the lesion as soon as possible. It is often a two-step process, done in conjunction with a Mohs dermatologic surgeon who ensures that the entire tumor has been excised at a microscopic level. Mohs’ surgery is a procedure developed specifically to remove a cancerous skin lesion, using visualization under a microscope to carefully remove the cancerous lesion layer by layer until all margins are free of any cancerous tissue. This technique spares as much of the surrounding healthy tissue as possible. Many of these eye fold defects can be sutured together directly, but many others may require more complex reconstructions. In many of these more complex cases, Dr. Taban may need to use adjacent tissues (what we call ”flaps”), or transfer of skin from other parts of the eye fold face or body (what we call “skin grafts”) to complete the reconstruction. Some of these more complex reconstructions may require more than one operation to complete (what we call “staged reconstruction”).


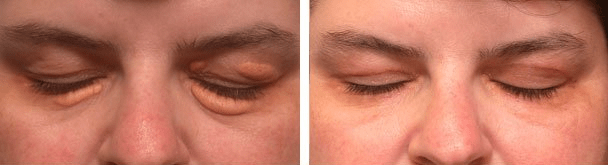
Before & After Photos
CONTACT THE LOS ANGELES OCULOPLASTIC EXPERT
Dr. Taban is one of the leading oculoplastic eye surgery doctors in the LA region. Contact us via online support form, or via telephone at: (310) 278-1836
After being diagnosed with a basal cell skin cancer on my eyelid, Dr Taban was referred via my dermatologist. The day of my reconstruction he presented me with multiple options and pros and cons … We didn’t know how skin was going to be removed from my eyelid until I had my cancer removed the day before his surgery to reconstruct it. He’s a great surgeon and you cannot even tell that I had half a dime-sized piece of skin cut off my eyelid…